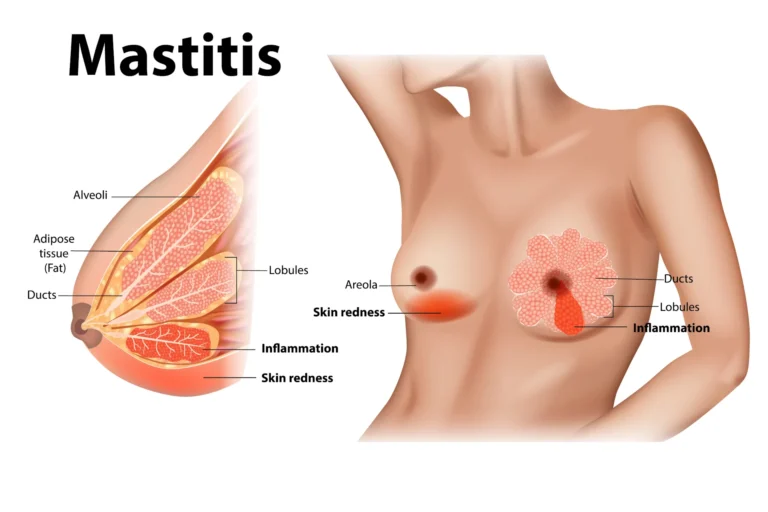
Mastitis is a painful infection of the breast that many nursing women have to face at some point in their nursing experience. Most often, mastitis is preceded by a plugged duct or a crack in or trauma to the nipples. Mastitis can occur at any point while a woman is breastfeeding, but happens more frequently during the early post-partum period. This is when the mother and child are establishing their breastfeeding routine. Mastitis is believed to be caused by germs entering the breast through the nipple.
Types of Mastitis:
- Non-infectious mastitis – this is usually caused by breast milk staying within the breast tissue – milk stasis – because of a blocked milk duct or a breastfeeding problem. If left untreated, the milk left in the breast tissue can become infected, leading to infectious mastitis.
- Infectious mastitis – this is caused by bacterial infection. It is important to receive treatment immediately to prevent complications, such as an abscess in the breast.
Causes of Mastitis:
Mastitis can occur when bacteria commonly found on the skin enter the nipple through small cracks. The bacteria then multiply in the fatty tissue of the breast surrounding the milk ducts (areas of the breast that produce milk), causing swelling, warmth, or pain. The swelling can press on the milk ducts and block them.
Chronic Mastitis: Women who aren’t breastfeeding and may be postmenopausal can develop chronic mastitis. In this case, the milk ducts below your nipple become inflamed. Your milk ducts can become clogged with dead skin cells and other debris.
Mastitis Risks Factors:
A risk factor is something that increases your chance of getting a disease or condition.
Risk factors include:
- Previous mastitis
- Abrasion or cracking of the breast nipple
- Wearing a bra or clothing that is too tight
- Missed breastfeeding (causing overdistention of the breast)
- Irregular breastfeeding
- Pressure on the breasts, caused by:
- Sleeping on the stomach
- Holding the breast too tightly during feeding
- Baby sleeping on the breast
- Exercising (especially running) without a support bra
- Anything that causes too much milk to remain in the breast, including:
- Baby’s teething
- Use of artificial nipple or pacifier
- Incorrect positioning of the baby during feedings
- Abrupt weaning
- Yeast infection of the breast
- Low resistance to infection or immune deficiency disorder
- Psoriasis or other skin conditions that affect the nipple
- Diabetes mellitus
- Rheumatoid arthritis
- Use of cortisone drugs
- Prior breast surgery or implants
Symptoms of Mastitis:
Infection of the breast by the bacteria Staphylococcus aureus causes symptoms which can mimic a clogged milk duct or an abscess. Unlike a clogged duct, mastitis does not go away on its own or by massaging the affected area. You may experience these symptoms whether you are breastfeeding or not. In mastitis, the symptoms do not usually resolve without intervention either in breastfeeding technique or by taking antibiotics.
The most common symptoms include:
- Breast lump
- Breast pain
- Breast redness and heat
- Breast swelling on the affected side only
- Fever and flu-like symptoms
- Itching
- Nipple discharge
- Nipple tenderness
- Tender or swollen lymph nodes in the armpit on the affected side
- Tenderness
Diagnosing Mastitis:
To determine if you have mastitis, your doctor will perform a physical examination and ask you about your symptoms. No tests are usually required for breast-feeding women.
However, if you are not breast-feeding, your doctor may request certain tests to better understand your condition. These may include mammography or a biopsy.
Treatment of Mastitis:
Mastitis treatment usually involves:
- Antibiotics: Treating mastitis usually requires a 10- to 14-day course of antibiotics. You may feel well again 24 to 48 hours after starting antibiotics, but it’s important to take the entire course of medication to minimize your chance of recurrence.
- Self-care remedies: Resting, continuing breast-feeding and drinking extra fluids can help your body overcome the breast infection. Empty the milk from your affected breast frequently. If your baby refuses to nurse on the affected breast, use a breast pump or hand express the milk to empty your breast.
- Adjustments to your breast-feeding technique: Making sure that you fully empty your breasts during breast-feeding and that your infant latches on correctly are key to avoiding bouts of mastitis. Your doctor may review your breast-feeding technique with you or may refer you to a lactation consultant for help and ongoing support.
If your mastitis doesn’t clear up after taking antibiotics, check back with your doctor. A rare form of breast cancer — inflammatory breast cancer — can also cause redness and swelling that could initially be confused with mastitis. Your doctor may recommend a diagnostic mammogram, and you may need a biopsy to make sure you don’t have breast cancer.
You Might Also Like:
- Top 9 Women’s Health Issues (Most Common)
- Polycystic Ovary Syndrome or PCOS: Best Diet Plan
- 14 Very Early Signs of Pregnancy
- Breast Augmentation: Its Types, Preparation And Surgery Process
- Tips to Get a Beautiful and Sexy Figure
- Breast Augmentation: Its Side Effects, Results And Cost
Mastitis prevention:
If you’re pregnant or nursing, practice good hygiene, avoid wearing bras that are too tight and try to prevent cracked nipples or treat them once they occur. Not letting too much time pass between breastfeeding will also help prevent clogged milk ducts. And always make sure you fully empty your breasts during feeding and that your infant latch is correct to avoid further mastitis. See a lactation consultant for support with your breastfeeding technique.